A new home-monitoring system at Richmond Hospital is keeping chemotherapy patients connected with doctors and nurses.
The hospital recently launched its Remote Symptom and Patient Monitoring System (RESPONSe) program, a mobile and web browser application that allows patients receiving treatment to self-report when they get home how they feel after each session.
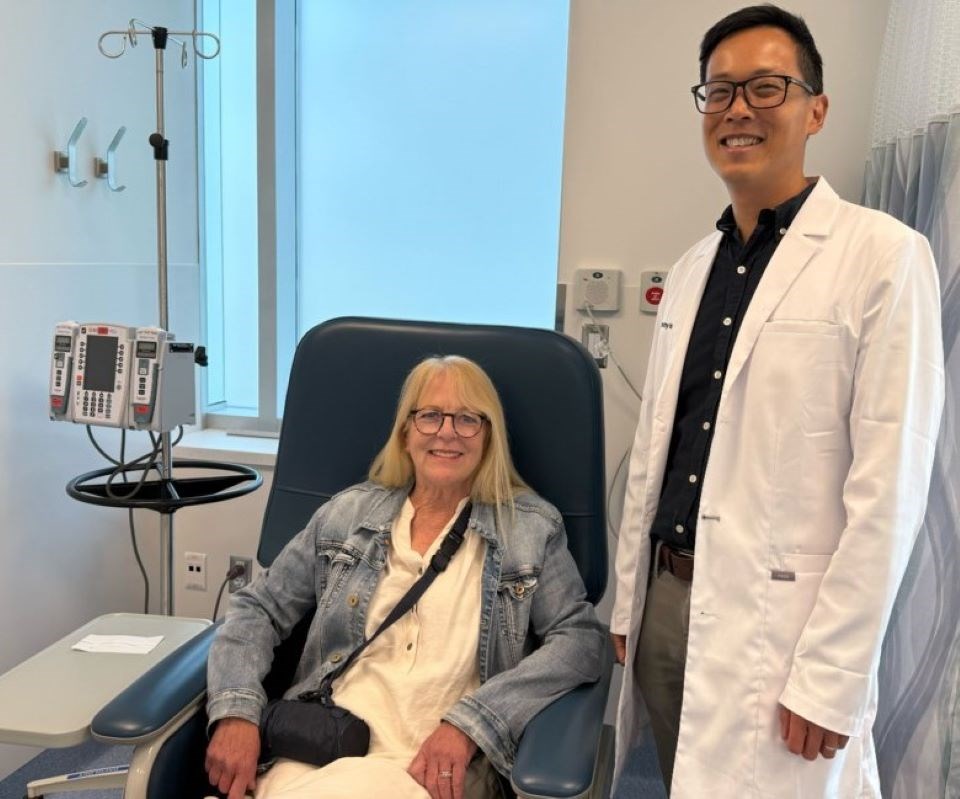
The purpose of the program is to reduce symptom burdens in patients, and for nurses and doctors to address concerns before they get worse, explained Dr. Jeremy Ho, medical oncologist and program lead at Richmond Hospital.
He told the Richmond News they were inspired by similar programs in the U.S. that build strong communication between patients and doctors.
"When there's better communication, patient symptoms are often better and possibly even visits to the emergency room are less," said Ho.
Planning began three years ago and this included getting B.C. Ministry of Health and Vancouver Coastal Health grants, gathering a team and building the system.
The program officially launched in January 2024, and now 150 Richmond Hospital patients are using the program.
Tsawwassen resident Sydney Cuthill, 65, is one of the hospital's Cancer Care Clinic patients who participated in the program and described it as "life-changing."
Cuthill was diagnosed with cancer after a hysterectomy in 2017 and has been battling cancer for the last eight years.
She received four rounds of chemotherapy and has since had her bladder and colon removed.
Doctors later told her the cancer had spread to her peritoneal area within her abdomen, and she returned to the hospital for chemotherapy again.
"I was dreading (chemotherapy)," said Cuthill, adding she became very sick, had hives and even lost her appetite.
She was introduced to the new RESPONSe program in February last year and said, "Anything that's going to help is a good thing."
How the RESPONSe program works
Patients who join the program have access to the system during their first six months of IV chemotherapy at Richmond Hospital's Cancer Care Clinic.
After a patient gets treatment, they are asked to complete a short survey through their phone, tablet or computer to tell doctors and nurses how they're doing or if there are any symptoms they need to pay attention to.
"If you were feeling all right, you wouldn't need to go further into the survey, but other times, if I wasn't feeling well or (I was) more tired ... it would delve into more information," explained Cuthill. This included adding both physical or mental symptoms.
After questions are answered, a dedicated nurse reviews the submitted survey and answers, and if issues or concerns are spotted, they will reach out to the patient to provide advice, arrange prescriptions or ask them return to the hospital to see a doctor.
While the monitoring program is accessible by patients from home, it is only available on weekdays during clinic hours.
"It would be really nice if we had 24 hours, seven days a week coverage," said Ho, adding, however, they're looking at how they can fill the current gaps.
Bridging communication gaps between patients and medical practitioners
The highlight of the program for many patients, including Cuthill, is the ability to communicate with doctors and nurses outside the care clinic.
"This program changed my life," said Cuthill.
"It feels like you have support, whereas, before I had no one to be able to call."
It was comforting knowing she could reach a nurse seamlessly five days a week when she had concerns, that she wasn't alone and was supported.
"I just so believe in it, and I think it can really help a lot of people coming through the clinic. It made me feel that much better. I hope it gets expanded throughout B.C."
Richmond Hospital's cancer care clinic nurses have made more than 700 phone calls to patients who need help dealing with symptoms at home, according to Ho.
He described the program as a "nurse in a pocket" where they can help their patients beyond the medical doors in a meaningful way.
"In the past, we relied on the patient to try to recognize in themselves if this is a serious side effect or not. But, of course, someone who's never gone through it, it's very hard to know if it's serious," said Ho. Before, they found patients only called when "things got really bad."
"This approach tries to be more proactive, and we're trying to catch symptoms much earlier and deal with them sooner so they don't turn into those serious issues."
Not only that, he added, it has prevented unnecessary visits to the emergency department.
A traditional Chinese language version of the program was also recently launched for Chinese-speaking patients.
The program is only being used at Richmond Hospital, but VCH has "visibility on it," said Ho.
"It'd be really nice to see this approach be used in other places, but that would not be under my control."
The hospital has received overwhelmingly positive response from patients who have gone through the program, and they have told Ho they feel reassured knowing that "help is not really far away."
"With that peace of mind, people can be confident going through treatment, knowing that they'll get help when they need it."
📣 Got an opinion on this story or any others in Richmond? Send us a letter or email your thoughts or story tips to [email protected].
📲 To stay updated on Richmond news, sign up for our daily headline newsletter.
💬 Words missing in article? Your adblocker might be preventing hyperlinked text from appearing.