It’s believed that one in five Canadians is bothered by it every day. It causes emotional, social and financial burden. It’s costing the nation tens of billions of dollars each year. And, it’s resulted in Canada being the second largest per-capita consumer of prescription opioids (hydrocodone, oxycodone, morphine, codeine) in the world, according to the International Narcotics Control Board.
“It” is chronic pain; a wide-ranging disorder caused by various factors that experts in the field say is grossly underfunded and barely recognized by the Canadian medical system.
And without a change in how pain is managed, the disorder is only going to get worse as Canada’s population ages; roughly two in three seniors suffer from chronic pain.
But how to heal or at least manage pain is a multi-faceted, multi-disciplinary approach that needs to be done on an individual basis. It requires commitment from the pain sufferer and an open-minded community of health practitioners.
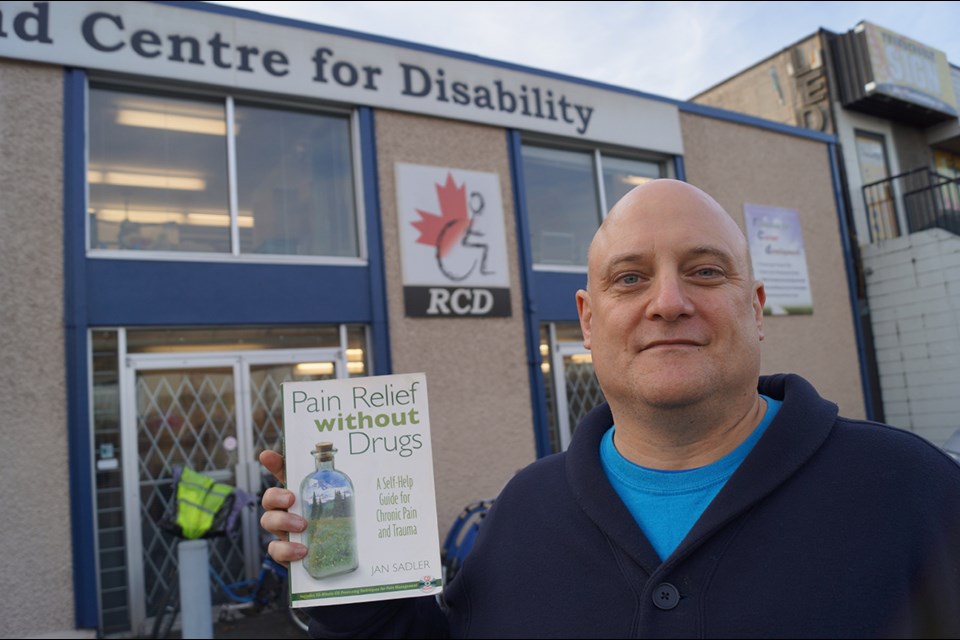
Dave Thomson, an education coordinator for the Richmond Centre for Disability (RCD), is on the frontlines of pain management in Richmond.
Thomson, 48, has fibromyalgia, a disorder that causes body pain and usually results in chronic fatigue syndrome.
“Sleep is the big thing. I don’t get much sleep. It’s clicking years off my life, I’m certain of that. I get about four hours of sleep in total,” said Thomson, who is presently running disease self-management courses at RCD, an organization that operates largely thanks to community grants and volunteers.
Thomson has, through the years, developed coping mechanisms for his pain. While he used to take several Tylenol and codeine pills daily, he is now weaning off a less powerful morphine patch.
“I can sleep in pain, I can dream in pain, I can fall asleep in a position that no one would dare consider because my brain will process the pain and not wake me up,” said Thomson, almost with a chuckle.

Costs to society
One of the province’s leading researchers of chronic pain, Dr. Marc White of the University of British Columbia, defines pain as an unpleasant sensory and emotional experience associated with actual or potential tissue damage.
“Chronic pain covers a great realm,” said White, who was a postdoctoral fellow at the Arthritis Research Centre of Canada.
White says academic studies show that arthritis — the most well known form of pain — costs roughly $30 billion a year in Canada when one adds up medical bills, lost wages, and missed economic opportunities. Overall, the Canadian Pain Society believes pain costs Canada closer to $40 billion.
“We are talking about a multi-billion dollar impact from pain on society,” said White.
White said pain is not just a physical symptom, it’s also a mental one.
“It doesn’t necessarily have to be a physical injury, which comes back to this whole notion of body and mind,” said White.

Body, mind, spirit
White noted chronic pain sufferers frequently experience mental side effects due to drugs. They may also become reclusive, leading to anxiety when entering society. In the worse cases, people become depressed and a cycle of pain and mental illness kicks in.
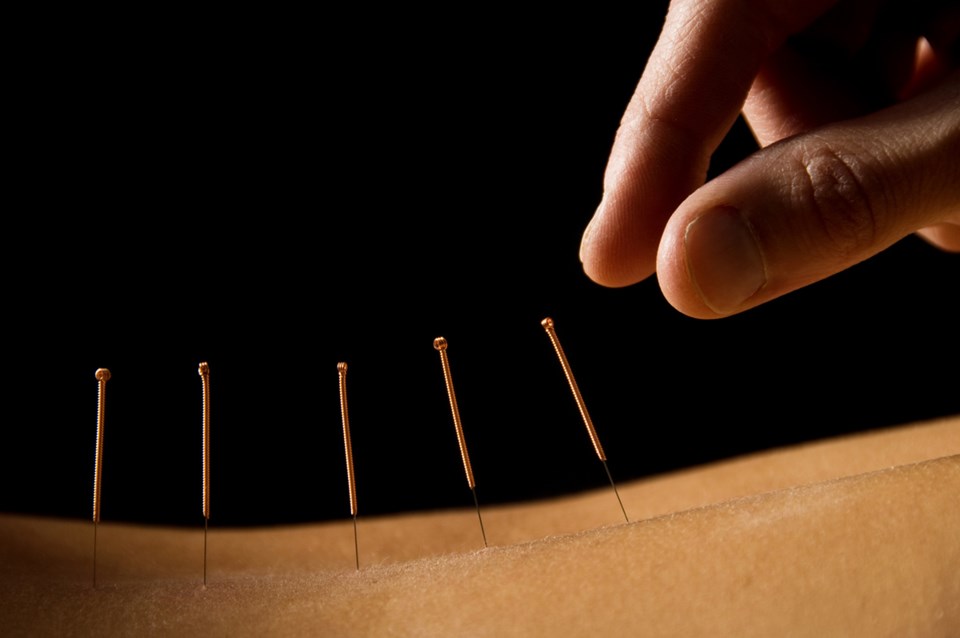
There are several methods of treatment for chronic pain. Drugs are probably the most well-known and frequently used method (simply taking Tylenol or Advil, for instance), but there is also the likes of physical treatments (acupuncture, massage therapy and chiropractic), psychological treatments (cognitive behavioural therapy and group therapy), as well as self-awareness treatments (energy healing, mindfulness meditation and yoga), all of which can blend together.
Finding the right treatment(s) can take years to find, said White.
“Each has their place. Part of the challenge is finding a combination of these things that help you cope and manage pain but may also have some restorative power,” he noted, adding that self-management techniques are crucial as well.
“It can be as simple as a hot bath that can relieve pain,” he said..
As with Thomson and his ability to sleep through pain, White said pain may never go away.
“For people with chronic pain it’s about getting to a place where we’re accepting pain, but in a special way. The pain changes and your experience of pain changes as you refocus,” said White.
A big problem, however, is the Canadian medical system’s lack of integrated services, not to mention financial pressures. Thomson said he realized family doctors either don’t understand the true scope of the issue and/or don’t have enough time to properly address every issue.
Drug-dependent system disjointed

Not only are doctors swamped with patients, the system, according to White, is disjointed.
“The problem the Canadian health care system has is, if you don’t have an extended health care plan, drugs are really the only method of pain relief that physicians are able to provide you with,” he said.
As such, opioid use in Canada has more than doubled since 2000, medical research indicates. According to Industry Canada, from 2001 to 2013, total pharmaceutical sales nearly doubled to $22 billion per year. And while there are no national data trends, Global News, citing Ontario Coroner data, reported opioid related deaths had tripled from 2002 to 2013.
Some health experts have reportedly called for a national strategy on prescription medication abuse. White said he wants to see a national strategy for pain management, as well.
White doesn’t dismiss the need for medications. Rather, he sees pharmacists as a vital process to pain management, especially in ensuring safe drug interactions and preventing abuse.
B.C.’s Medical Services Plan does not insure costs for the likes of psychologists, counsellors, physical or massage therapists, acupuncturists and natural healers, all of which cost at least $100 per session.
Vancouver Coastal Health has an insured pain clinic at St.Paul’s Hospital, but the wait time is approximately one year.
Massage therapy is one of the most popular methods of pain relief utilized by those with medical insurance.
Physical therapies, according to Michael Henniger, a registered massage therapist at Steveston’s Turning Point Wellness Centre, have the advantage of treating the root medical cause of the pain as opposed to pharmaceutical interventions that simply mask it.
“Massage therapy has many different benefits, both physical and mental. It helps with posture, muscle imbalances, tension, range of motion, anxiety, depression and much more,” said Henniger.
But he also acknowledged that whatever method one chooses, it has to be the right one for the individual.
“I find that a lot people view their pain as part of life. It’s just something they deal with on a day-to-day basis. What they need to learn is that there are many ways to help manage that pain. Getting the right treatments can help alleviate the pain and in some case remove it all together,” he said. Even if you can’t afford frequent visits, a massage therapist can educate you on home pain relief and prevention methods, such as a stretching routine.

Sedentary life a culprit
Henniger said it’s our ever-increasing “sedentary lifestyles” that have contributed to the chronic pain epidemic.
“Driving, sitting at a desk, watching television on the couch; all these things are detrimental to the body and over time can lead to chronic pain,” he said.
The rush of day-to-day life is also having well-documented adverse affects on people’s mental health. So, healing the mind may be just as important as healing the body. Depression and anxiety is “part and parcel with a lot of this stuff,” said Thomson.
Natural healing and self-awareness exercises are other healing methods that are becoming increasingly mainstream as society becomes more aware of the harmful effects of overusing medications.
Natural healer Sudha Devi practices various methods of healing such as mainstream Western-Eastern practices, which includes breathing therapy and yoga, as well as more traditional Eastern practices such as Marma therapy and Jin Shin Jyutsu, both of which involve opening energy channels in the body through the application of slight pressure on control points of the body.
Devi uses such Eastern practices and Western scientific research to heal the mind and body. She conducts one-on-one treatments from her home office in Steveston and late last year she established the Richmond People in Pain Network Support Group that meets monthly at the Richmond Caring Place Society.
For Devi, also a sufferer of fibromyalgia, managing chronic pain is a deep, emotional, individual experience. But it need not be a lonely one, which is typically the case.
“No one knows your pain,” she said.
“When we start talking, there is a diagnostic process which we start. One level is pain but the other levels are mental and emotional,” she said. “When you start sharing (your experience) something happens because you know someone else feels like you do. They’re not judging you. And at our meetings you can lie down if you want, because we know how you may be feeling.”
Devi said when a person is injured, say in a car accident, energy pathways can be blocked. By taking daily moments for the likes of yoga or breathing exercises, or simply just channeling positive thoughts while resting, she believes people can at least come to terms with their pain. This can also help stop the vicious cycle of pain and depression, she said.
And when that happens, other healing methods such as drugs or overt physical treatments can become more effective.
“Self healing is not a quick fix …you will still have anxiety but it won’t stop you from participating in things,” she said.
White says natural healing methods are not new but our understanding of how they may affect chronic pain is.
"What is new is research using brain scans and a new understanding of the neuroplasticity and how pain gets modulated through different ways,” said White.
Essentially, scientists are discovering the interplay between emotions and the brain’s chemistry that affects pain receptors.
Thomson, White and Devi noted that there’s another important aspect to pain management — family support. UBC Associate Professor of Psychology Susan Holtzman studies pain and families.
She said loved ones often under or over estimate others’ pain, which can lead to ignorance of the issue or smothering and a resultant lack of independence for the patient.
It’s important to remember that there is no one “right way” to provide support. Much of this comes down to communication,” she says.
Communication is why Thomson invites family members to his workshops.
Too much information
Another important social aspect to pain management is to understand that as easily as one may find a particular treatment that works, one can also become over burdened with different treatments and recommendations from others.
So, be careful, White warned. “Sometimes one can get over treated,” he said.
And, noted Thomson: “You don’t want to go crazy. You don’t want to go to the other edge. If you go on the Internet you can be smothered with information.”
Yes, get knowledgeable about your illness but focus on your basic health,” he says.